Hallux valgus is a bony deformity at the base of the big toe, characterized by a lateral deviation of the toe and a painful protrusion of the metatarsophalangeal (MTP) joint. While non surgical treatments like orthotics or footwear modifications may alleviate symptoms, surgery is often recommended for severe cases.
Common Causes of Hallux valgus
Hallux valgus due to a combination of genetic, biomechanical, and environmental factors:
1. Foot Structure : Inherited foot shapes, such as flat feet or hypermobile joints, increase susceptibility.
2. Footwear : Tight, narrow, or high heeled shoes force the toes into unnatural positions, accelerating deformity.
3. Arthritis : Inflammatory conditions like rheumatoid arthritis weaken joint stability.
4. Trauma or Overuse : Repetitive stress from activities like ballet or sports may contribute.
Symptoms Necessitating Surgery
Surgery is considered when conservative treatments fail to address:
Persistent Pain : Aching or sharp pain at the MTP joint, worsened by walking.
Reduced Mobility : Stiffness limiting daily activities.
Visible Deformity : Severe toe misalignment causing overlapping toes or corns.
Chronic Inflammation : Swelling and redness unresponsive to rest or medication.
Types of Bunion Surgery
The surgical approach depends on the deformity’s severity, patient age, and lifestyle. Common procedures include:
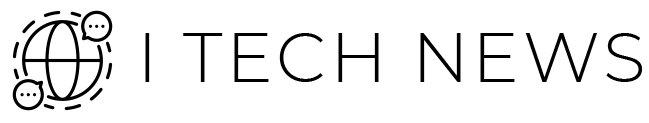
1. Osteotomy
Incision: A longitudinal incision is made over the medial aspect of the first metatarsophalangeal (MTP) joint.
Bone Reshaping :
Chevron Osteotomy : A “V” shaped cut at the metatarsal head to realign the bone.
Scarf Osteotomy : A “Z” shaped cut in the metatarsal shaft for moderate to severe deformities. The distal fragment is shifted laterally to correct the intermetatarsal angle (IMA).
Fixation : Titanium screws or plates (e.g., Herbert screws) are used for stabilization.
Soft Tissue Balancing : Adjuvant procedures like Akin osteotomy (phalangeal wedge resection) or lateral soft tissue release may be combined.
2. Arthrodesis
Cartilage Removal : The damaged cartilage of the MTP joint is excised to expose subchondral bone.
Joint Alignment : The first metatarsal and proximal phalanx are positioned in 10–15° of dorsiflexion and neutral rotation.
Fixation : Compression screws (e.g., cannulated screws) or dorsal plates (e.g., Arthrex) are applied for rigid fixation.

3. Exostectomy
Minimal Incision : A small medial incision is made over the bony prominence.
Bone Resection : The medial eminence (骨赘) is removed using a micro osteotome or high speed burr
Soft Tissue Repair : May include medial capsulorrhaphy (tightening) or lateral release.
Limitations : Does not correct toe alignment; often combined with osteotomy.
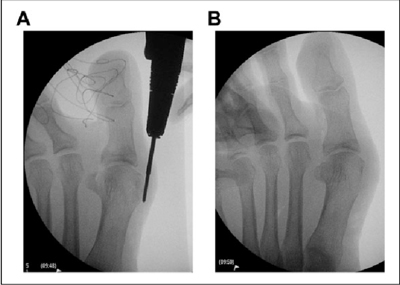
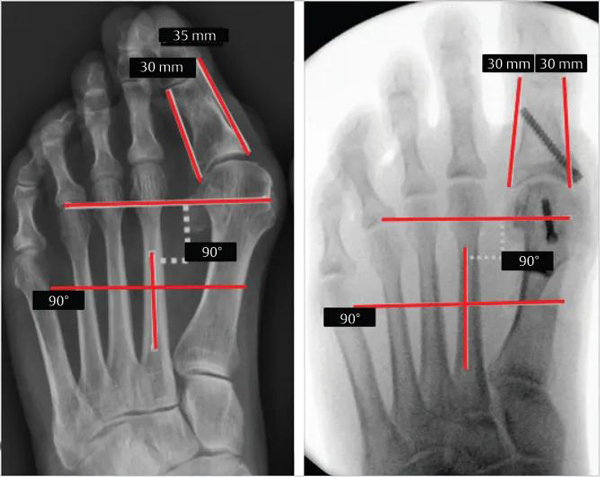
4. Minimally Invasive Surgery (MIS)
Mini Incisions : 2–3 incisions (<5 mm) on the medial and lateral sides of the MTP joint.
Bone Correction :
Percutaneous Osteotomy : A burr (e.g., Shannon burr) or specialized saw is used for metatarsal or phalangeal cuts under fluoroscopic guidance.
Lateral Release : The adductor hallucis tendon is released through a lateral incision.
Fixation : Headless compression screws or absorbable pins are inserted.
Advantages : Faster recovery (2–4 weeks) but limited to mild deformities.
Surgical Efficacy and Outcomes
Studies show 85-90% of patients experience significant pain reduction and improved function post surgery. Key outcomes include:
Pain Relief : Most report diminished discomfort within 3 months.
Cosmetic Improvement : Toe alignment is restored in >80% of cases.
Recurrence Risk : 5–10%, often due to improper footwear or underlying biomechanics.
Recovery Tips :
Elevate the foot and ice to reduce swelling.
Avoid tight shoes; use orthotics to maintain correction.
Physical therapy enhances strength and flexibility.
Bunion surgery effectively addresses pain and deformity when non surgical methods fail. While recovery requires patience, advancements in techniques like MIS have improved outcomes. Consulting a foot specialist ensures personalized treatment, balancing anatomical needs and lifestyle goals.